Example of Nursing Notes: Essential Templates & Tips

Nursing notes are a critical component of patient care, providing a detailed record of observations, interventions, and outcomes. They ensure continuity of care, facilitate communication among healthcare teams, and serve as legal documentation. Whether you’re a seasoned nurse or a student, understanding how to write effective nursing notes is essential. Below, we explore essential templates, tips, and best practices to help you master this skill.
Why Nursing Notes Matter
Nursing notes are more than just paperwork; they are a reflection of patient care quality. Accurate and detailed notes help in:
- Tracking patient progress
- Identifying trends or changes in health status
- Ensuring legal compliance
- Facilitating interdisciplinary collaboration
Well-structured nursing notes also save time and reduce errors, making them indispensable in clinical settings.
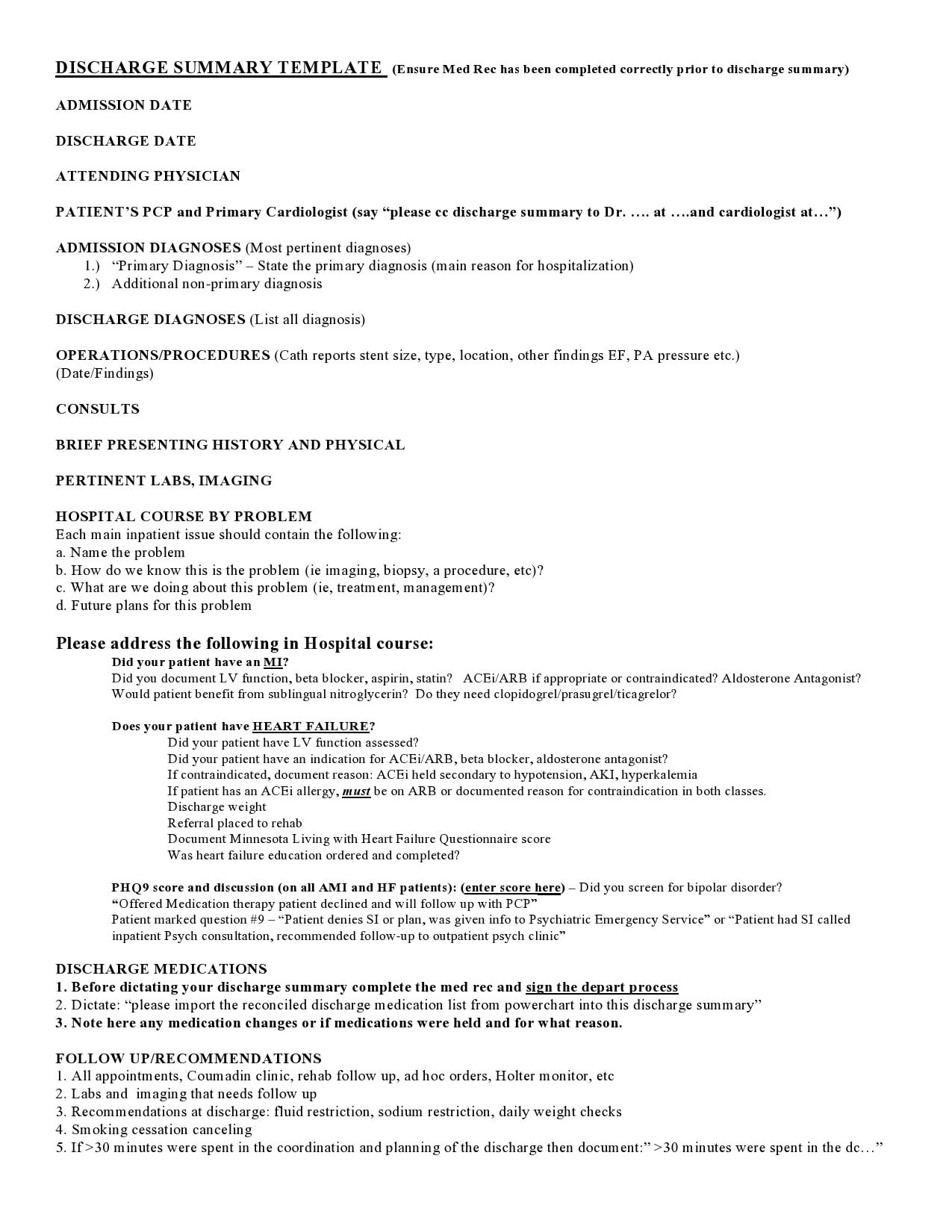
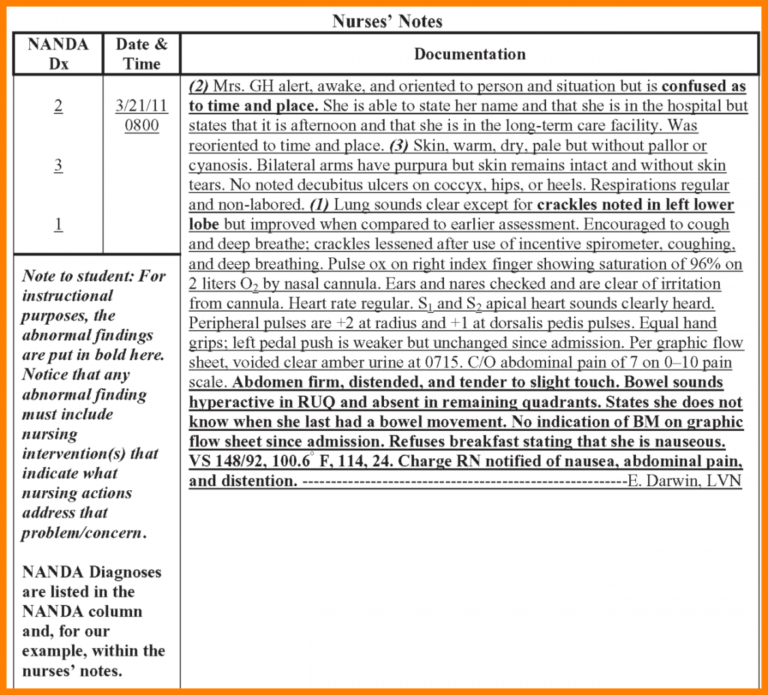
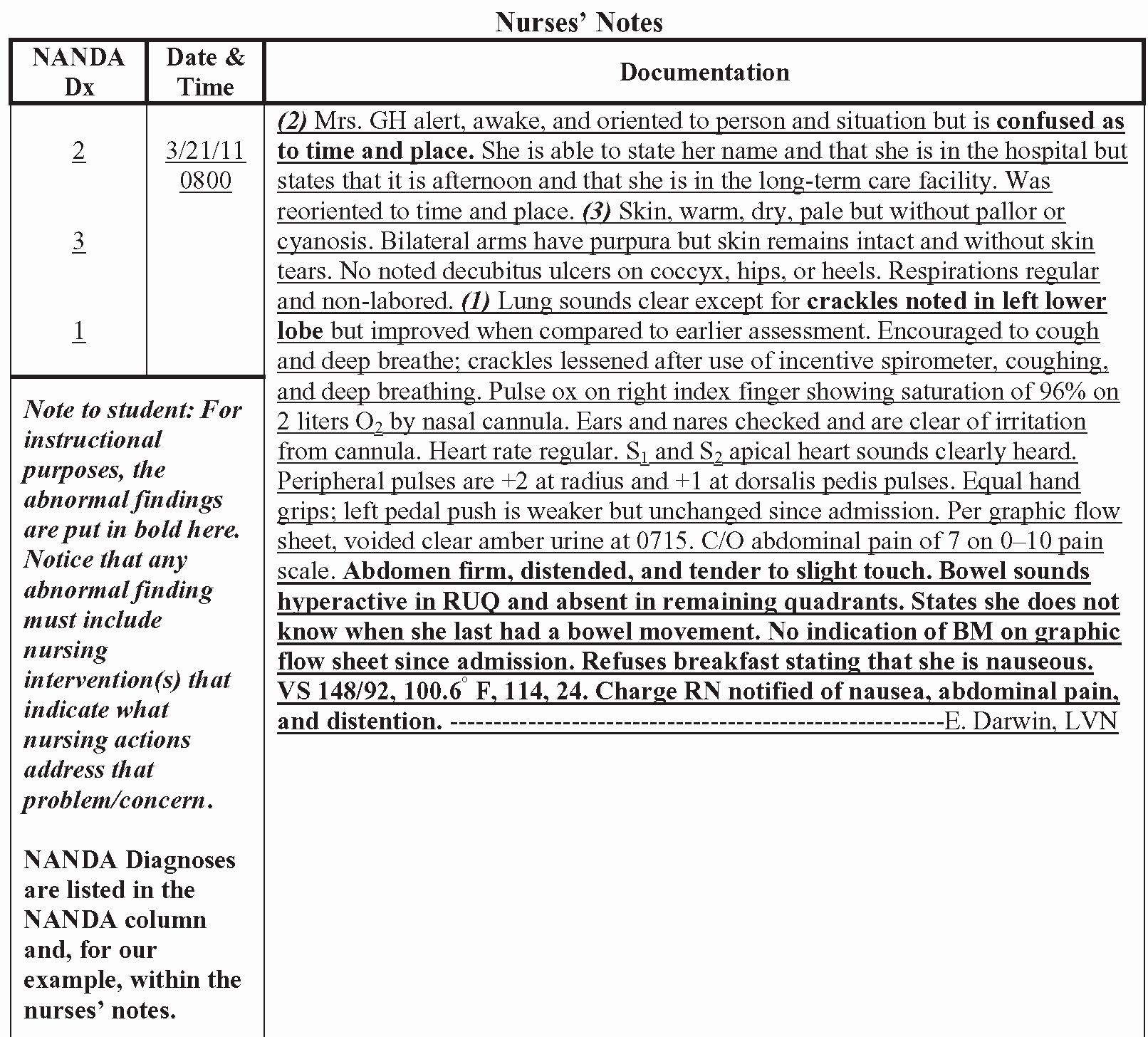
Essential Components of Nursing Notes
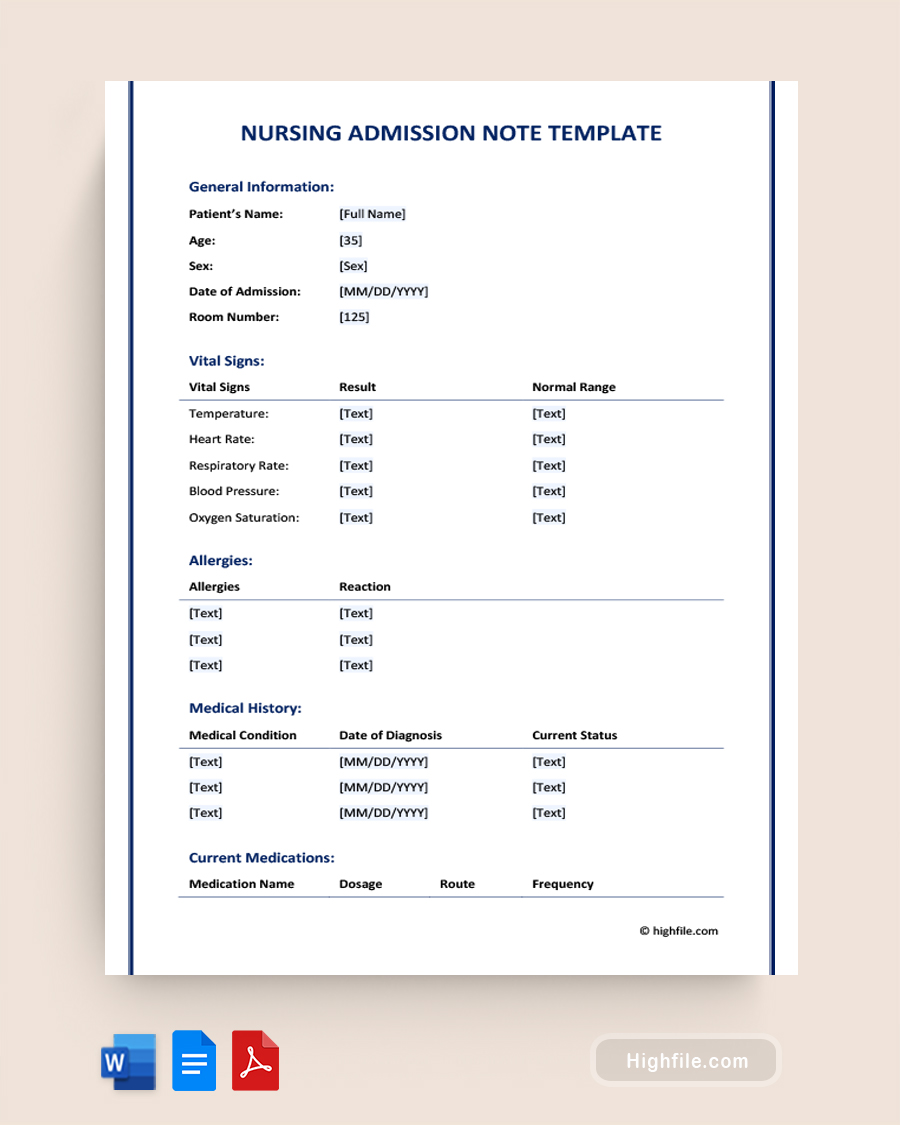
Every nursing note should include the following elements:
1. Patient Information: Name, age, and unique identifiers.
2. Date and Time: Record when the observation or intervention occurred.
3. Objective Data: Measurable facts (e.g., vital signs, lab results).
4. Subjective Data: Patient’s feelings or symptoms (e.g., “reports severe pain”).
5. Nursing Interventions: Actions taken (e.g., administered medication, provided education).
6. Outcomes: Patient response to interventions.
7. Signature: Your name and credentials.
📝 Note: Always use clear, concise language and avoid medical jargon when possible.
Example Nursing Note Templates
Below are two commonly used templates for nursing notes:
SOAP Note Template
S (Subjective): “Patient reports difficulty breathing.”
O (Objective): “Oxygen saturation at 88% on room air.”
A (Assessment): “Suspected respiratory distress.”
P (Plan): “Administered oxygen at 2L/min and notified physician.”
DAR Note Template
D (Data): “Patient’s blood pressure is 160⁄100 mmHg.”
A (Action): “Administered prescribed antihypertensive medication.”
R (Response): “Blood pressure decreased to 140⁄90 mmHg after 1 hour.”
| Template Type | Best Use Case |
|---|---|
| SOAP | Comprehensive patient assessment |
| DAR | Quick documentation of interventions and outcomes |
Tips for Writing Effective Nursing Notes

- Be Concise: Stick to relevant details.
- Use Standard Abbreviations: Ensure they are universally understood.
- Avoid Bias: Focus on facts, not assumptions.
- Update Regularly: Document changes promptly.
- Proofread: Ensure accuracy and clarity.
✨ Note: Regularly review your notes to maintain consistency and accuracy.
Checklist for Perfect Nursing Notes
- [ ] Include all essential components (patient info, date/time, etc.).
- [ ] Use a structured template (SOAP, DAR, etc.).
- [ ] Document objectively and subjectively.
- [ ] Sign and date every entry.
- [ ] Review for clarity and accuracy.
Nursing notes are a cornerstone of patient care, ensuring that every detail is captured and communicated effectively. By using the right templates, following best practices, and maintaining consistency, you can create notes that enhance patient outcomes and streamline workflows. Remember, clear and accurate documentation is not just a requirement—it’s a reflection of your professionalism and commitment to care.
What is the SOAP note format?
+SOAP stands for Subjective, Objective, Assessment, and Plan. It’s a structured format for documenting patient assessments and care plans.
How often should nursing notes be updated?
+Nursing notes should be updated after every significant patient interaction or change in condition.
Can I use abbreviations in nursing notes?
+Yes, but only use standard, universally understood abbreviations to avoid confusion.
nursing documentation,nursing templates,SOAP notes,DAR notes,nursing best practices